Prevention is the best medicine and often the cheapest.
A recent article[1] by the ABC cited that two new Hepatitis C medications, which were approved and listed on the Pharmaceutical Benefits Scheme (PBS) in March 2016, cost the Australian taxpayer close to $943 million in four months and provided just 43,943 prescriptions.
When considering these figures it’s easy to see why these drugs have already taken the top two spots on the list of Australia’s most expensive medications.
Hepatitis C is a very serious disease that they estimate kills over 400,000 people annually[2]. A blood borne pathogen, its transmitted through coming into contact with infected blood. With over 230,000 Australians recorded to be carrying Hepatitis C, the health system are only less than a fifth of the way through treating current recorded cases with these new drugs, meaning tax payers could spend at least another $5.5 billion on this medication alone in the coming years.
The development of these drugs, and their inclusion on to the PBS was a welcome relief to sufferers. As although this medication severely impacts the recipients health and well being during the month long course of treatment, often leaving a patient bedridden, it actually has a 90-95% chance of curing the disease.
This is unlike other drugs previously used to treat Hepatitis C, which do not cure the disease and mean a lifetime of being on medication that also negatively impacts lifestyle and well-being to varying degrees.
The problem is these new drugs are incredibly expensive. Due to this, in many parts of the world they are not a viable option for treatment, and in Australia, it’s the taxpayer that foots the lion’s share of the bill.
If you do the math, this $943 million dollar spend providing 43,943 prescriptions means that it’s a cost of $21,455.63 per person. 90-95% of this money has been well spent, but still, it’s a lot of money. Money that could be used elsewhere if we can prevent these infections.
Further to this, up to this point we have only talked about dollars spent on the actual medication. Underneath this upfront expense lie a number of other hidden costs. This includes the loss of skilled and productive members of the workforce. Often these patients are unable to work while taking the medication due to the severe side effects while undergoing the treatment. Then there is also the personal cost to their life up to this point, their state of mind and health, the cost of counselling and the cost of recovery. None of these are calculated in financial terms but can all add up to millions.
These are just the basic statistics and figures for Hepatitis C.
The reality of the matter is that there are over 20 blood borne pathogens that we know to worry about. Every one of these diseases represents significant ongoing financial and community costs.
Surely there is a better way?
One of the most common ways to be infected with a blood borne pathogen, and one of the most preventable, is through the transmission of infected blood via a needle or infected sharp medical device.
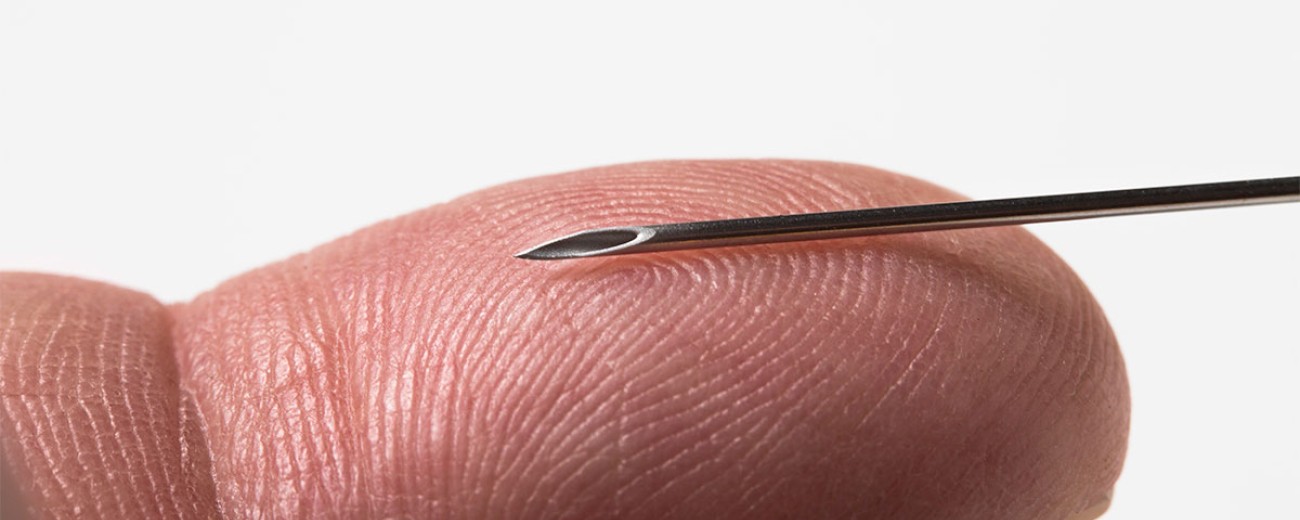
In recent years new technology has been developed to create a variety of safe medical devices and needles that protect against needle stick injury and the re-use of needles, therefore preventing the spread of blood borne disease.
As always there is some resistance to the adoption of new technology and new processes within any industry and this instance is no different. However, the use of this technology as a way of preventing the spread of blood borne pathogens is gaining momentum and acceptance in the medical fraternity and represents a viable solution to the problem these diseases present.
Recently[3] the World Health Organisation (WHO) stated that by 2020 they want every hospital and clinic to use only “smart syringes” that are designed so they reduce the risk of needlestick injury and can’t be used more than once. They rightly claim that the use of these sorts of safety syringes would reduce the spread of deadly blood-borne diseases.
In a study undertaken in 2010 by the WHO, re-used needles accounted for 1.7 million new hepatitis B cases, tens of thousands of new HIV infections and hundreds of thousands of new hepatitis C infections each year globally. That was 10 years ago. With more people in the world today it stands to reason that these numbers are now worse.
When looking closer to home, it is estimated that in Australia there are 30 needlestick injuries per 100 hospital beds per year and that at least 18,000 Australian healthcare professionals suffer from needlestick injuries per year[4]. These numbers are alarming and staggering. It is also worth considering how much goes un-reported and then tripling these figures – at least!
What is so frustrating is that all of this cost and damage to the safety of the community is preventable with current and available technology. That’s why the WHO thinks smart syringes are worth it, even though they cost at least twice as much as traditional needles.
The cost of manufacturing each syringe per unit is more expensive than a traditional syringe, there’s no denying it. However, the immediate, Whole of Life Cost together with the long-term savings of the use of this technology must surely be taken into account to get a real view of the costs, savings and benefits.
These savings include: the reduced need for the treatment of people infected with blood borne pathogens. These costs are massive in today’s world and growing with every new infection. They include: initial testing to understand if an infection is present; expensive and ongoing medication; the drain on medical resources and services to treat these people (even if it is done ‘in house’); loss of work and productivity; the mental state and well being of the person infected and the personal cost of this; the risk of these people infecting others; and the general cost of safety to the wider community.
It is often said that you get what you pay for and in this circumstance the mounting evidence suggests that the cost of a more expensive syringe is mitigated many times over by the long term savings of its use.
Also tied up very closely in this issue is the universal question of worker safety. In Australia, worker rights and safety are protected by legislation. Globally it’s getting to be the same. This technology works towards preventing the chance of needlestick injury and the reuse of the same syringe. Its focus is on the safety of the health worker, the patient, the user and the community as a whole. It’s about prevention of the spread of these diseases.
And surely preventing a problem if the technology and resources are available is always a better option that treating it after the damage has been done.
We have the technology, lets use it properly and invest in all of our safety.
Numedico Technologies is an Australian-based wholesaler of the ClickZip™ Needle Retractable Safety Syringe, the highest quality manual retractable needle injectable delivery system in the Asia-Western Pacific region. Its mission is to provide access to truly functional, practical and safe medical devices.
The ClickZip™ Needle Retractable Safety Syringe is a new and globally patented Swiss technology active, high quality needle with a retraction mechanism, thus preventing needlestick injury and syringe reuse.
It is one of the best safety syringes on the market today and is able to be manufactured at a fraction of the cost of many of its competitors.
Ideal and safe for many applications including: large-scale immunisation programmes; hospitals; and medical clinic applications.
Footnotes
[1] http://www.abc.net.au/news/2016-12-05/hep-c-drugs-australias-most-expensive/8094188
[2] https://www.osha.gov/SLTC/bloodbornepathogens/index.html
[3] https://www.evernote.com/shard/s445/nl/76456195/4c24e7b1-c709-486c-930f-6066c5018a2e/
[4] https://www.mtaa.org.au/sites/default/files/uploaded-content/website-content/Sharpsv5.pdf
Articles reference in the writing of this blog:
Subscribe to Numedico News.




